What is Diabetic Retinopathy?
Diabetes mellitus, commonly known as diabetes, is a metabolic disorder characterized by elevated blood sugar levels due to a malfunction in insulin secretion. If not controlled, it can have destructive effects, especially on the eyes, kidneys, and nervous system. There are two types of diabetes. Type 1 is often seen in childhood, while type 2 is usually seen in individuals over the age of 40. Type 2 diabetes accounts for 90-95% of diabetics.Diabetes is among the top three diseases that cause blindness. The retina, known as the layer of nerves in the eye responsible for light sensitivity and vision, is affected by this complication of diabetes due to the prolonged damage to small blood vessels in the retina caused by high blood sugar levels. Blockages in small vessels, malnutrition, new vessel formation, and bleeding occur.
About 2% of diabetics develop blindness and 10% develop severe vision loss within 15 years of diabetes duration.
What are the Risk Factors for Diabetic Retinopathy?
The most important risk factors include the duration of diabetes and blood sugar levels. Other risk factors include genetic factors, high blood pressure, high cholesterol levels, obesity, smoking, and lack of physical activity. The risk of developing retinopathy also increases during pregnancy.How is Diabetic Retinopathy Diagnosed?
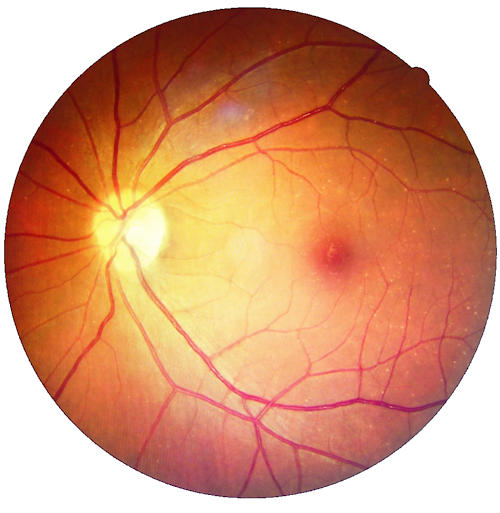
It is possible to detect the presence of retinopathy through dilated fundus examination after applying pupil-dilating drops. Imaging techniques such as Fundus Fluorescein Angiography (FFA) and Optical Coherence Tomography (OCT) provide valuable information for determining the presence and degree of retinopathy, determining the treatment approach, and evaluating the response to treatment.OCT is a non-invasive imaging method that scans the central vision in thin sections using laser and provides valuable information in evaluating the presence of edema in the macula, membrane formation on the macula, and the presence of macular holes. It is also used to evaluate the response to treatment.
FFA is a non-radiating angiography performed by injecting contrast material into the patient's arm to better examine the retinal vascular structure. It is a very useful method for detecting areas of non-perfusion in the retina or choroid layer, new vessel formations on the retina or optic nerve, and leaking vessels.
How is Diabetic Retinopathy Treated?
After the diagnosis of diabetes, routine check-ups for retinal follow-up are very important.Control of blood sugar levels, blood pressure control, monitoring cholesterol levels, and avoiding smoking are general precautions that can be taken. It is recommended that the average blood sugar level over 3 months, known as HbA1c, be below 7.
In the presence of retinopathy, treatment options include laser treatments, intraocular Anti-VEGF and steroid applications, and surgical procedures.
- Argon laser treatment; reduces new vessel formation by applying it to ischemic areas of the retina, and increases retinal oxygenation.
- Anti-VEGF and steroid applications; applied to the vitreous cavity of the eye. It is applied under local anesthesia in sterile conditions. They are effective in regressing or eliminating new vessel formations on the retina and optic nerve. They are also effective agents in regressing edema developed in the macula, known as the central vision. With regular injection applications, it is possible to preserve vision and increase visual acuity.
- Surgical treatment (vitrectomy); is a method applied in advanced stage retinopathy in the presence of intraocular hemorrhages, in the presence of membranes that contract and shrink the retina surface, in the presence of detachment with tears and detachment in the nerve layer. During the surgery, depending on the condition of the eye, air, gas, or silicone can be given into the eye as a tamponade after surgery. The aim is to achieve a retina with normal anatomy and a functionally improved eye in terms of visual acuity. Successful results can be achieved with early surgical intervention.
How Should Diabetes be Monitored?
- Symptoms of diabetes typically begin to appear about 5 years after the onset of the disease.
- Even if there are no symptoms, it is recommended that diabetic patients undergo an annual examination.
- Patients with mild retinopathy symptoms should undergo examination every 3-4 months.
- Examination is recommended at the end of the first 3 months of pregnancy.
- Early and intensive treatment and close monitoring are crucial for treatment success.




